One of the challenges for India and for other developing countries is the fact that much of medical humanities (MH) has come from and is influenced by the West. Cultures …
Shared Commentary: An Argument in Favor of Reading Our Missing Hearts and All Our Names as a Paired Assignment
I read all the time. But vacations are still special. I look forward to stuffing two or three books into the side compartment of my suitcase and having the extra time and freedom to read over the next week or two.
The Awakening
I waited patiently to cross the road. There were long lines of cars punctuated by occasional motor bikes that do not always follow the rules; the line seemed never-ending.
Interview with Anne Stiles, Ph.D., on Christian Science, ‘Mind Cure,’ and Children’s Literature
Anne Stiles’ most recent book, Children’s Literature and the Rise of “Mind Cure” examines the confluence of religion and health within the context of children’s fiction.
Interview with JOEL SHULKIN, Physician/Writer
Joel Shulkin, MD is an author and practicing physician. A 1999 graduate of New York University School of Medicine, He is currently in the practice of developmental behavioral pediatrics.
Howling Basset Books Comes to Rural New Jersey
Zohar Kfir and Lisa Lynch recently opened Howling Basset Books, a brick-and-mortar bookstore, in an old Victorian house in Oldwick, New Jersey.
“Hunger Pains: Andrew Mangham, Ph.D., on Medicine & Starvation in Victorian Literature”
As the founder and director of the Centre for Health Humanities and a professor of English at the University of Reading, UK, Andrew Mangham, Ph.D., has published extensively on medicine and Victorian literature.
Interview with Carla Joinson, author of Vanished in Hiawatha: The Story of the Canton Asylum for Insane Indians.
Carla Joinson is an independent scholar based in Church Hill, Tennessee. Published in 2016 by the University at Nebraska Press, Joinson’s Vanished in Hiawatha: The Story of the Canton Asylum …
Interview with Jim LeBrecht, co-director of Crip Camp
Students in the Medical Humanities elective at the NYU Grossman School of Medicine had the opportunity to interview Jim LeBrecht, co-director of the Oscar nominated documentary Crip Camp. The …
Interview with John Hoffman, Co-director of Fauci
In February 2022, students enrolled in the Medical Humanities elective at the NYU Grossman School of Medicine, met with John Hoffman to discuss Fauci, a 2021 documentary he co-directed with Janet Tobias on the life and work of Dr. Anthony Fauci.
Being a left-hander in a right-handed world
During the good old days, especially among Asians, writing with your left hand was a big ‘taboo’. The teachers of yore were strong believers in corporal punishment …
The Virtual Salon: Book Clubs During 2020 at NYULH
When thinking about these last two years, I can’t help but think of books. Just as with each aspect of our lives, as an avid reader, what I’ve read (or not read), how I’ve read it, and who I’ve read it with has been deeply impacted by the events of 2020.
The Masked Identity
Some countries in East Asia were already using masks during the SARS epidemic and started using them quickly during the current one. I am struck by the stark differences in the acceptance and use of face masks globally.
Quarantined!
The process of COVID testing was going smoothly. People were paying the fees, completing the required paperwork, and getting swabbed. I had just landed in Kuala Lumpur, Malaysia from New Delhi, India, and the process was a mandatory part of the arrival formalities along with a two-week quarantine
Reading Foucault’s The Birth of the Clinic in 2021: Does the Gaze Still Dominate its Masters?
“This is a book about space, about language, and about death; it is about the act of seeing, the gaze,” Michel Foucault writes opening The Birth of the Clinic (p. ix).
Healing her…..healing me….
“There are career-defining moments that support the sacrifice, the stress, the trauma, the sleep deprivation, the juggle, and everything in between in child abuse pediatrics practice.”
Taking a Shot: An Interview with Daniela J. Lamas, MD, on the Covid-19 Vaccination
The narrative captures a range of emotions following your Covid-19 vaccination. There is a dual sense of relief and ephemerality as you sit in the hospital’s waiting room for the fifteen-minute post-vaccination period. You reflect on your patients, illness, mortality, and the hope that the vaccine affords. What was unusual about these fifteen minutes? What made this period reflective?
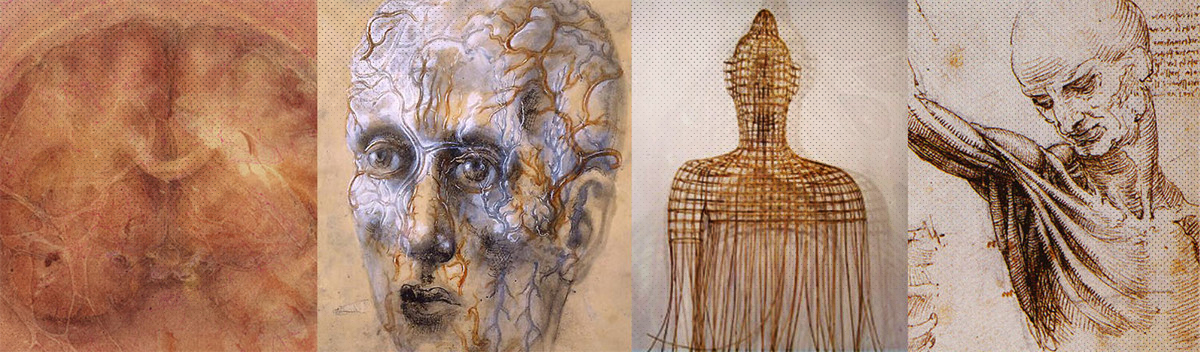
Stanley B. Burns M.D. Historic Medical Photography Collection Acquired by Yale
The Stanley B. Burns M.D. Historic Medical Photography Collection was recently acquired by the Harvey Cushing/John Hay Whitney Medical Historical Library at Yale University.
Using Visual Thinking Strategies (VTS) to Enhance Interprofessional Education
“I wish your husband came to me 5 years earlier.” That’s what the Whipple surgeon said to me after my husband was diagnosed with pancreatic cancer. From 2010-2016 my husband was in and out of the hospital 40-50 times.
The Past, Present, and Future of Medical Television
No matter who you are or what your profession, anyone who has lived in the United States during the past eight decades has witnessed the tremendous popularity of medical television shows over the years.
Being Patient
I was feeling bitterly cold. The shivering did not stop. Unintelligible voices began coalescing into words. Words joined into sentences.
The Betrothed During the 2020 Pandemic
The Betrothed, a novel written by Alessandro Manzoni and first published in 1827, is an expression of the author’s interest in early seventeenth-century Italian history in the form of an accurate, literary explication of historical events, religious life, and social structures in the northern regions of the country at that time.
Sealed in!
May evenings in Mumbai, India are hot and sticky. You are always drenched in sweat and the wet heat is decidedly uncomfortable. Ceiling fans make ineffectual attempts to dissipate the enervating heat.
Reading Arrowsmith During the 2020 Pandemic
By J. Russell Teagarden Reading the 1925 novel Arrowsmith during the 2020 coronavirus pandemic reveals many parallels that can make us wonder if the outcomes of pandemics will forever be …
Memories of the Spanish Flu
My time spent in the army now seems to me like a long, complex dream. The events are all familiar, but you cannot be sure whether they really happened. After a very brief period of basic training in New Jersey, I was stationed in South Carolina as a physician at a small army base.
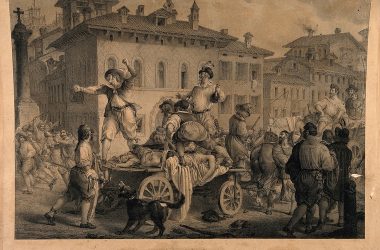
Medicine as spectacle: Public expectations of physicians as seen through art and television
If “all the worlds a stage,” then the operating theater is no different. Surgeons of the Renaissance and nineteenth and early twentieth centuries, despite the modern day medical profession’s emphasis on privacy, stoicism, and quiet dignity, were historically required, not only to heal, but to entertain.
Editor’s Choice
Dr. Gabriel Redel-Traub‘We Have No Superpowers’: A New Doctor’s Lessons From the PandemicDr. Gabriel Redel-Traub is one of 52 members of the NYU Grossman School of Medicine Class of 2020 …