2018 marks the 100th Anniversary of the Spanish Flu epidemic. As we endure one of the toughest flu seasons in years, Jacalyn Duffin, MD, PhD, a hematologist, historian and LitMed Database editor talks about the significance of the 1918 event and what is in store for the future.
Briefly describe the Spanish Flu Pandemic in 1918.
Why was it “Spanish”? What made it so notable?
At the end of World War I, influenza swept the globe in a devastating pandemic that affected an estimated 500 million people and killed 20 to 50 million–more than the number of deaths attributed to the recent war (up to 11 million military and up to 6 million civilians).
Influenza may have originated on hog farms in the American mid-west and circled the world twice before Spain announced that it had a problem. Throughout the late 19th and early 20th centuries in the various attempts to create international sanitary commissions, countries were loath to declare outbreaks of infectious disease for two main reasons: it would make them vulnerable to attack during conflicts, and it would provoke fear among trading partners leading to decline in exports. Spain had been a non-combatant during the war and spoke up first. Consequently, it is unfairly called ‘Spanish.’
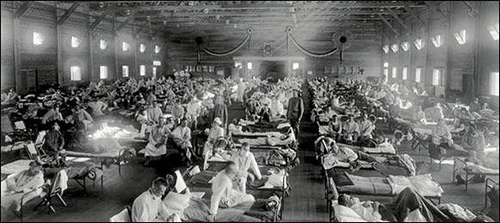
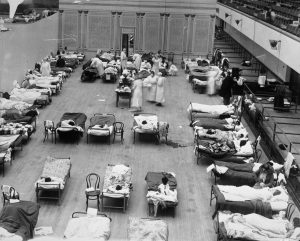
The infection had a predilection for young people–who may not have had the natural immunity triggered by contact with earlier outbreaks. It was especially prevalent among those occupying crowded spaces: soldiers in barracks, students in dormitories. Its danger stemmed from an associated pneumonia.
Treatment at that time was supportive: fluids, cooling with baths and salicylates, and agents to promote expectoration. There were no specific drugs to cure it.
In trying to control and prevent influenza, public-health authorities closed places of public gatherings, such as schools and theaters; they cancelled concerts and discharged all but the sickest patients from hospitals. A crackdown on insalubrious behaviors–such as spitting and coughing – was mediated through public awareness campaigns. People were encouraged to wear masks to protect themselves and others.
Among the most effective measures for containing influenza was (and still is) quarantine, a method that dates back to the fourteenth-century plague in Europe. The sick and contacts with them are kept isolated for a specified time, which is determined by trusted information about the incubation period and duration of the infection.
Why are we marking the 100th Anniversary?
Influenza is a cautionary tale. It destroyed many families with loss of young people in the prime of their lives. It reminds us of our constant vulnerability to new and emerging pathogens in nature.
The causative agent of influenza, though suspected of being a virus, was not known in 1918. Its identification is intimately linked to the scientific and technological history of infectious disease Consequently, influenza serves as a reminder of several scientific achievements.
First, it prompted clarification of the nature of viruses. Germ theory had been articulated in the early 1880s, and by 1918 many diseases such as tuberculosis, syphilis, gonorrhea, cholera, diphtheria, typhoid, whooping cough, and various pneumonias, were already linked to bacteria–microorganisms that were visible under the light microscope. These bacteria could be eliminated by filtration–at least in the laboratory.
But by 1892, scientists had also learned that some pathogens passed right through the filters: these were viruses–not bacteria–and they caused rabies, polio, and smallpox. In 1917, Félix d’Herelle announced his discovery of an “invisible antagonistic microbe” that attacked the bacteria causing dysentery: he called it a “bacteriophage” (eater of bacteria) or “phage.” Phages are viruses that attack bacteria. For some time, researchers hoped that they might provide a form of therapy against microbial diseases in humans.
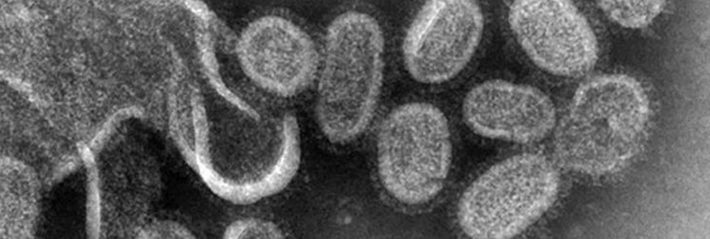
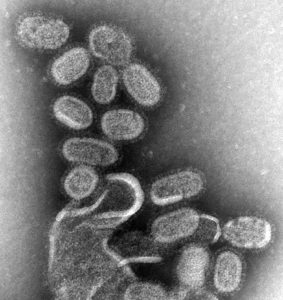
Viruses could not actually be visualized until the advent of the electron microscope in the 1930s. Influenza virus was isolated and identified in 1933.
Second, influenza is also a reminder of the mid-century development of genetics, which provided a new way of characterizing pathogens. It is caused by many different yet related viruses. Nevertheless, they are all single-stranded RNA viruses, together with many other pathogens for diseases such as the common cold, Hepatitis C, Ebola, polio, and measles.
Finally, influenza reminds us of the development of technologies and drugs for treatment. Beginning with the iron lung, used in the polio outbreaks and the smaller, more portable endotracheal models that we use today, mechanical respirators can save lives by “breathing” on behalf of the sick, keeping them alive until the pneumonia subsides, and their lungs heal. As for drugs, the best-known anti-viral is oseltamivir (Tamiflu) originally derived from the Chinese star anise plant, which has a long history in Chinese and Ayurvedic folk medicine. It was approved for use in the USA in 1999. Anti-viral drugs are helpful but are thought to be only weakly effective against some viral strains.
Has there been anything like it since that time?
Influenza returned as “the Asian flu” in 1957, which left one to two million dead. At that time, it was possible to show that it was a different strain of virus from the culprit in 1918. The “Hong Kong influenza” pandemic in 1968-1970 killed up to four million.

A threatened outbreak in 1976 prompted President Gerald Ford, on the advice of scientists, to recommend a massive vaccination campaign. But the vaccine resulted in the side effect of an increase in the usual number of cases of Guillain Barré Syndrome (ascending paralysis). Furthermore, the threatened epidemic did not have the predicted severity. The campaign was stopped. The episode shook confidence in vaccines among the general public.
In looking for comparators, historians also consider the nature and management of outbreaks of diseases that are not caused by influenza virus, but just as easily transmitted and carry a high morbidity and mortality: for example, polio in the mid-twentieth century, Ebola, SARS, and Zika. Management of these outbreaks relies to a certain extent on the same quarantine methods laid down seven centuries ago.
The AIDS epidemic is often invoked in these discussions; however, HIV behaves differently from flu virus: the incubation period is much longer, the illness protracted, and the spread limited to direct contact with body fluids. These characteristics meant that, unlike influenza, HIV could spread widely before it was detected.
Is the flu of today similar to the one that circulated in 1918?
How is it different?
The symptoms are essentially the same. Differences reside in virulence, which depends on the type and strain of the virus provoking the outbreak.
There are three types of human influenza, called A, B and C. The fourth, type D, affects animals. The most virulent, type A, is classified on several parameters including the types of molecules it contains: H (hemagluttinin) and N (neuramidase). Recent outbreaks and threatened epidemics of various forms of influenza A have dominated the news, making the public aware of terms such as H1N1, H3N2, H5N1.
What led up to the development of the first vaccines?
Why do they change every year?
Are we anywhere near a universal vaccine? What are the obstacles?
By 1918, vaccines had already been produced for several diseases now known to be viral. For example, smallpox was prevented by using variola (smallpox) in the 1720s and possibly much earlier, and with vaccinia (cowpox) by Edward Jenner in 1796. Louis Pasteur developed a rabies vaccine in 1885. These successful precedents, coupled with the virulence of the 1918 pandemic, prompted a search for an effective vaccine against influenza.
At first, scientists attempted to make vaccines from various bacteria, assuming that the deadly pneumonia was an additional super-infection; however, these vaccines were ineffective because the assumption was incorrect.
The first influenza vaccine in the US was licensed for military use in 1945 and for civilian use in the following year. The US army has been vaccinated annually since that time. However, in the first applications, the effectiveness was reduced by the advent of a different viral strain from Australia, not covered by the first vaccine.
When the 1957 epidemic occurred, scientists discovered that most survivors of the 1918 flu had no antibodies against this new influenza virus. This finding helped them to classify it as a different variety of influenza, now known as H2 whereas the 1918 influenza was a strain of H1N1.
One of the biggest problems in producing influenza vaccine is the fact that the virus changes frequently and rapidly. Consequently, new vaccines have to be elaborated each year based on epidemiological information about the predominant strains.
In the United States and Canada, annual vaccination against influenza is voluntary. But with better predictors of viruses and rapid preparation for vaccines, public health authorities now support campaigns that encourage vaccination. These efforts often target high risk groups: pregnant women and the elderly. Beyond the tragic human cost of a severe epidemic, they believe that the expenses of these campaigns–even with free vaccination–are well justified in contrast to the tremendous financial burden of widespread illness.
2018 promises to be a significant flu season, although not a pandemic. Reports from early January indicated that the vaccine for this year was prepared from a virus that has since mutated in the wild, or had mutated in the lab. Therefore, it did not offer the promised degree of protection.
At the time of writing a universal vaccine for influenza, though much discussed, seems to be far in the future.
Are we likely to see another outbreak like the one in 1918 or one that’s even worse?
Yes. Thanks to organizations, such as the World Health Organization, international notification should come more quickly so that the problem can be identified and contained. But pathogens are constantly evolving.
One theory – about the “pathocenosis,” which originated with physician-historian Mirko Grmek–would imply that our control over some pathogens with vaccines and drugs leaves a “space” for new ones to enter.
What would be different this time around?
The virus would be quickly identified and characterized–as was the case with SARS (which is caused by a coronavirus).Effective biological agents, such as the drug Tamiflu, would also be used to treat cases, and severely affected people could be kept alive with the use of respirators.
But caregivers know that maintaining adequate, fresh stocks of antiviral drugs is difficult and expensive, especially as time passes and the threat is forgotten: many outdated supplies must be thrown away and replaced. Furthermore, a severe outbreak could quickly mobilize all the respirators available. They worry about panic over access to care.
Containment of the outbreak will rely on ancient methods of barrier technologies (masks), handwashing, covering coughs and sneezes, and quarantine.
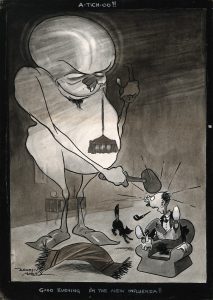
What captured the imagination of writers and artists about this epidemic?
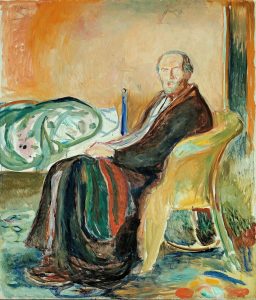
Influenza has been an important topic for writers. Our database contains more than twenty entries that relate wholly or in part to influenza–fiction, non-fiction, poetry and film (see Appendix).
The majority explore 1918 influenza in the United States–but other places and types of viral problems also appear. The high mortality, the predilection for the young, and the pervasive gloom of the great epidemic are recurrent themes in this collection.
Please let us know of other works to add to our collection and tell us what you like about them. You can use the comments section below.
Bibliography
- Centers for Disease Control, Types of influenza viruses, September 2017.
- College of Physicians of Philadelphia, The History of Vaccines Timeline
- Alfred W. Crosby, “Influenza” in Kenneth Kiple, ed. Cambridge World History of Human Disease (Cambridge and New York: Cambridge University Press,1993), pp. 807-811.
- Pietro Crovario et al., History and evolution of influenza vaccines. Journal of preventive medicine and hygiene 52.3 (2011): 91-4.
- John M. Eyler, The fog of research: influenza vaccine trials during the 1918-19 pandemic.
Journal of the History of Medicine & Allied Sciences. 64.4 (2009):401-28. - C. Franco-Paredes C et al., “H1N1 influenza pandemics: comparing the events of 2009 in Mexico with those of 1976 and 1918-1919.” Arch Med Res40.8 (2009): 669-72.
- Jean Paul Gonzalez et al., “Pathocenosis: A Holistic Approach to Disease Ecology.” Ecohealth 7.2 (2010): 237–41
- Mirko D. Grmek, Pathological Realities: Essays on Disease, Experiments, and History, ed. and trans. Pierre-Olivier Méthot. (New York: Fordham University Press, forthcoming August 2018)
- D.H. Kruger et al., “Helmut Ruska and the visualisation of viruses.” Lancet 355. 9216 (2000): 1713-7.
- David M. Morens, et al., “The 1918 influenza pandemic: Lessons for 2009 and the future.” Crit Care Med. 38.4 Suppl (2010): e10–e20.
- J K, Taubenberger et al., “1918 Influenza: the mother of all pandemics.” Emerg Infect Dis. 12.1 (2006); 15-22.
Appendix
Items about Influenza in the Literature Arts and Medicine Database
- In Flanders Fields, 1915 Poem
McCrae, John - I Have a Rendezvous with Death
Alan Seeger - Wickett’s Remedy, 2005 novel
Goldberg, Myla - They Came Like Swallows, Novel 1939
Maxwell, William - The Age of Grief, novella 1987
Smiley, Jane - A Day’s Wait, 1933 short story in 1987 collection
Hemingway, Ernest - The Desert Pilgrim: en Route to Mysticism and Miracles, memoir
Swander, Mary - Postcards of Nursing: A Worldwide Tribute, art 2004
Zwerdling, Michael - Bellevue: Three Centuries of Medicine and Mayhem at America’s Most Storied Hospital. nonfiction
Oshinsky, David - Osmosis Jones, film
Murray, Bill, Farrelly, Peter, Farrelly, Bobby - Bedside Manners, contains story Flu Shot, 2005
Watts, H. David - Blue Nights, memoir
Didion, Joan - The Virus, poem, 1994
Skloot, Floyd - Emerging infectious diseases cover art, 2003
Potter, P. & Drotman, D.P., eds. - The Great Influenza: The Epic Story of the Deadliest Plague in History, non fiction 2005
Barry, John - Deafening, novel 2003
Frances Itani - Five Days at Memorial: Life and Death in a Storm-Ravaged Hospital
Fink, Sheri - Lovesick, novel, 1997
Mastretta, Ángeles - Gilead, novel 2004
Robinson, Marilynne - Pale Horse, Pale Rider, short story 1990 collection
Porter, Katherine Anne - Kyrie, poems, 1995
Voigt, Ellen Bryant - The Last Town on Earth, novel 2005
Mullen, Thomas - Malade, 1916 poem in collection 1971
Lawrence, D. H. (David Herbert) - Cannery Row, novel 1992
Steinbeck, John