When I first watched The Knick two years ago, it seemed like a show about the past and the rapid pace of medical discoveries in the early days of modern medicine, before antibiotics
Category: The Artist Studio
States of Grace: From Doctor to Patient and Back Again
Before the accident, Dr. Grace Dammann was a caregiver through and through, in every aspect of her life. A pioneering AIDS specialist, she co-founded one of the first HIV/AIDS clinics for socioeconomically disadvantaged patients in San Francisco at Laguna Honda Hospital.
NYU Center for Humanities Event Imagining Illness: Pulitzer Prize Winners on Truth and Fact in Narrative David Oshinsky and Paul Harding
On a recent winter’s evening, Pulitzer Prize winners David Oshinsky and Paul Harding appeared together at the NYU Center for Humanities in an event cosponsored by the NYU Division of Medical Humanities and the Bellevue Literary Press.
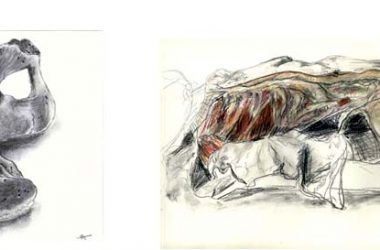
Cortney Davis – When the Nurse Becomes a Patient: A Story in Words and Images
NYU Langone Medical Center welcomed author/painter Cortney Davis to the Smilow gallery for the opening of “When the Nurse Becomes a Patient.” Laura Ferguson’s interview with Ms. Davis appears here. …
Rediscovering a history of trauma: An interview with Dr. Annita Sawyer
I’d been working full time for twenty years. As a psychotherapist I had reached a comfortable place professionally. My children were grown and on their own, so I had privacy.
Wherever You Go: Self-Representation and Williams Syndrome
Looking out over the dance floor at Nashville’s Wildhorse Saloon as other members of our group line danced with the crowd below, Mark told me “It’s good for us to get out into the community so that people know we exist.”
Cortney Davis – When the Nurse Becomes a Patient: A Story in Words and Images (Part II)
Part II of a dialogue between author and painter Cortney Davis and our Art Editor Laura Ferguson.
Cortney Davis – When the Nurse Becomes a Patient: A Story in Words and Images (Part I)
Part I of a dialogue between author and painter Cortney Davis and our Art Editor Laura Ferguson.
Thinking About the Body Through Visual Art
Readers of the Literature, Art & Medicine Blog may remember me as the first Artist in Residence at NYUSOM, or as the creator and teacher of Art & Anatomy in …