In February 2022, students enrolled in the Medical Humanities elective at the NYU Grossman School of Medicine, met with John Hoffman to discuss Fauci, a 2021 documentary he co-directed with Janet Tobias on the life and work of Dr. Anthony Fauci.
Being a left-hander in a right-handed world
During the good old days, especially among Asians, writing with your left hand was a big ‘taboo’. The teachers of yore were strong believers in corporal punishment …
The Virtual Salon: Book Clubs During 2020 at NYULH
When thinking about these last two years, I can’t help but think of books. Just as with each aspect of our lives, as an avid reader, what I’ve read (or not read), how I’ve read it, and who I’ve read it with has been deeply impacted by the events of 2020.
The Masked Identity
Some countries in East Asia were already using masks during the SARS epidemic and started using them quickly during the current one. I am struck by the stark differences in the acceptance and use of face masks globally.
Peaks and Valleys
House staff lecture today covers child maltreatment, and I compare and contrast cases of child neglect. Although reluctant, I feel obligated to include the reality of fatal neglect, with a slide of an intubated girl pictured from the bottom of her dirty feet up. The overriding message I hope is prevention—a chance to reflect on all of our efforts before neglect and abuse happen.
Quarantined!
The process of COVID testing was going smoothly. People were paying the fees, completing the required paperwork, and getting swabbed. I had just landed in Kuala Lumpur, Malaysia from New Delhi, India, and the process was a mandatory part of the arrival formalities along with a two-week quarantine
Reading Foucault’s The Birth of the Clinic in 2021: Does the Gaze Still Dominate its Masters?
“This is a book about space, about language, and about death; it is about the act of seeing, the gaze,” Michel Foucault writes opening The Birth of the Clinic (p. ix).
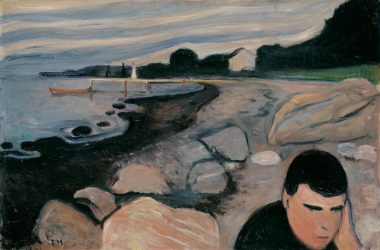
Edvard Munch: Painting the Soul
“If the soul is where feelings and emotions reside, then the soul is where the Norwegian expressionist painter, Edvard Munch, visited and is the source for many of his paintings.”
Rx Books: An Interview on Bibliotherapy with Darlina Liu
“Picture books are relatively low cost and accessible. They comprise an environmental tool that could be harnessed to support kids of parents with mental illness.”