“There are career-defining moments that support the sacrifice, the stress, the trauma, the sleep deprivation, the juggle, and everything in between in child abuse pediatrics practice.”
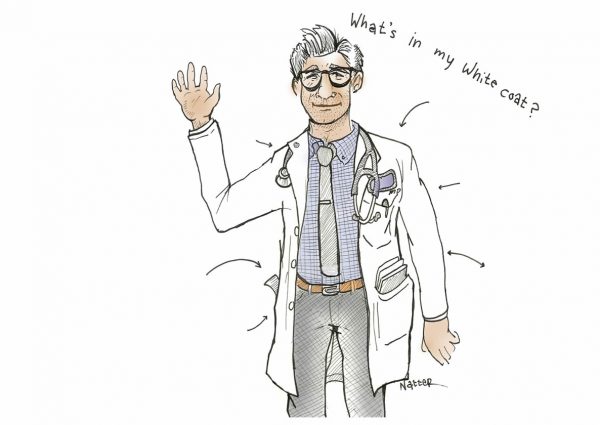
Taking a Shot: An Interview with Daniela J. Lamas, MD, on the Covid-19 Vaccination
The narrative captures a range of emotions following your Covid-19 vaccination. There is a dual sense of relief and ephemerality as you sit in the hospital’s waiting room for the fifteen-minute post-vaccination period. You reflect on your patients, illness, mortality, and the hope that the vaccine affords. What was unusual about these fifteen minutes? What made this period reflective?
Stanley B. Burns M.D. Historic Medical Photography Collection Acquired by Yale
The Stanley B. Burns M.D. Historic Medical Photography Collection was recently acquired by the Harvey Cushing/John Hay Whitney Medical Historical Library at Yale University.
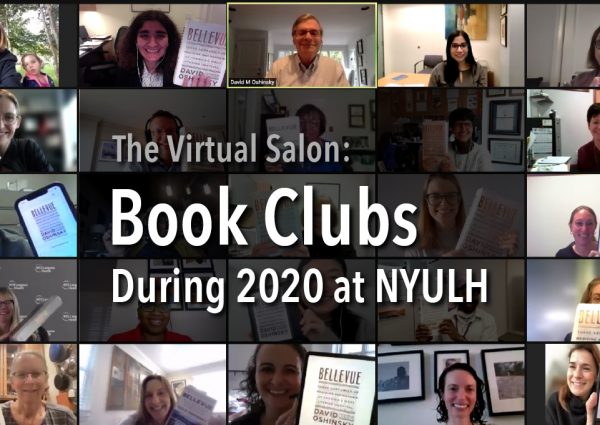
Using Visual Thinking Strategies (VTS) to Enhance Interprofessional Education
“I wish your husband came to me 5 years earlier.” That’s what the Whipple surgeon said to me after my husband was diagnosed with pancreatic cancer. From 2010-2016 my husband was in and out of the hospital 40-50 times.
The Past, Present, and Future of Medical Television
No matter who you are or what your profession, anyone who has lived in the United States during the past eight decades has witnessed the tremendous popularity of medical television shows over the years.
Being Patient
I was feeling bitterly cold. The shivering did not stop. Unintelligible voices began coalescing into words. Words joined into sentences.
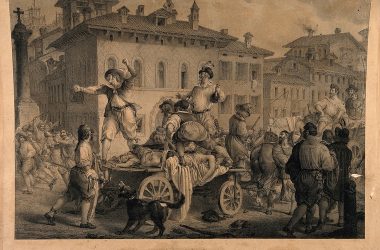
The Betrothed During the 2020 Pandemic
The Betrothed, a novel written by Alessandro Manzoni and first published in 1827, is an expression of the author’s interest in early seventeenth-century Italian history in the form of an accurate, literary explication of historical events, religious life, and social structures in the northern regions of the country at that time.
Sealed in!
May evenings in Mumbai, India are hot and sticky. You are always drenched in sweat and the wet heat is decidedly uncomfortable. Ceiling fans make ineffectual attempts to dissipate the enervating heat.
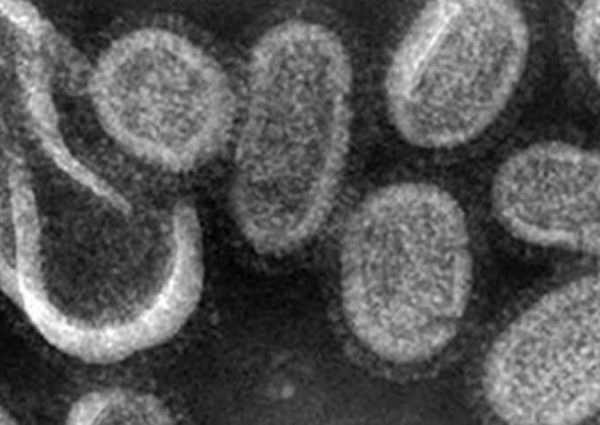
Reading Arrowsmith During the 2020 Pandemic
By J. Russell Teagarden Reading the 1925 novel Arrowsmith during the 2020 coronavirus pandemic reveals many parallels that can make us wonder if the outcomes of pandemics will forever be …