Commentary by Nancy Gross, MMH, MA, Palliative Care Community Liaison and Facilitator/Scholar of Humanities Programs, Overlook Hospital/Atlantic Health, Summit, New Jersey
“The humanities are the hormones…to infect with the spirit of the Humanities is the greatest single gift in education.”
Williams Osler, The Old Humanities and the New Science (1)
Humanities Programs at Overlook Hospital
Since 2005, Overlook Hospital has promoted programs in the humanities. This was not part of an institutional plan, but rather at the initiation of several humanities proponents and some willing administrators. These programs are stealthily flourishing in the midst of explicit campus, clinical and technological development.
1/2005-ongoing
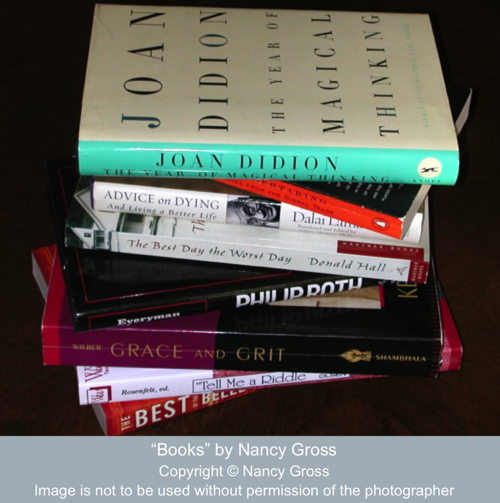
A monthly two-hour seminar series running from January to June with twenty hospital employees as participants. Overlook is one of seven New Jersey hospitals participating in the program which is supported in over twenty-five states. Participants include both clinical and non clinical health care professionals. Literary works evoking medical themes are read and discussed; books and a meal are provided. The goals of this national program are to increase caregiver empathy for patients, to improve patient-physician communication skills, to stimulate cross cultural awareness, to enhance job satisfaction, and to create community among professionals. Evaluative data are available for the national, state and Overlook cohorts. As of the 2008-09 academic year, the hospital’s division of Academic Affairs has assumed support of this program.
- Literature and Medicine: A Community Dialogue
9/2007-ongoing
A community based program modeled after the national hospital Literature and Medicine program. The program reaches 15-20+ participants per six month session, totaling four sessions during the grant period. The focus of this program is on educating participants around issues of aging, care giving, palliative care, medical decision-making, and end-of-life. Community response has been positive. The program has proven to be a powerful way to reach out to the community members in order to educate and empower them about the present day reality of medical institutions and end-of-life scenarios. This program has been generously supported by the Blanche and Irving Laurie Foundation.
- Narrative Medicine/Medical Humanities Conferences
10/2007-ongoing
A ninety-minute monthly conference for Internal Medicine residents in which a short literary work is presented. Residents and faculty read and discuss the work in light of their own daily practice as physicians. A short reflective writing session follows the discussion. Physicians share their work orally, and subsequently all edited writing is shared electronically. Physicians are encouraged to continue working on their pieces and to deposit their writing into their professional portfolios. Resident writing has appeared in hospital publications and research events.
- Conversations
9/2008-ongoing
A ninety-minute monthly conference with 3rd and 4th year medical students during their hospital clerkships. Students are introduced to the concept of narrative medicine and medical humanities philosophy and practice. They are presented with a short published piece written by other medical students. They discuss the piece, and relate it to their own experience as emerging physicians. Students write reflectively and share their writing, which is subsequently distributed to the group electronically.
- Film Night
9/2008-ongoing
A monthly film screening and discussion for residents and other hospital professionals that provides a relaxed and collegial atmosphere to de-stress. Classic and contemporary films that portray physicians and medical themes are shown. A discussion follows the screening.
- Literary Readings and Special Events
5/2008-ongoing
- Danielle Ofri, MD, PhD, physician/author read from her work Incidental Findings. Clinicians and community members attended
- Paul Gross, MD, physician/author /founding editor of PulseMagazine.com presented a rationale for physician writing and elicited short pieces from family practice and internal medicine residents
- Penny Harter, poet, read from Night Marsh to a mixed audience of health care professionals and community members
- Stephen Kiernan, journalist/author conducted a conference call to discuss his work Last Rites with Literature and Medicine: A Community Dialogue participants
- Rosemary McGee, poet, will read and discuss her work Spilling My Guts to Literature and Medicine at the Heart of Healthcare® participants
Proposed programs:
- A Night at the Movies at Overlook
A pending grant proposal to have a monthly film screening at Overlook for the neighboring community. The focus of the films and discussions will be around aging, caregiving, medical-decision-making, palliative care and end-of-life.
- Art Show and Lecture
Visit by Ana Blohm, MD to show her photographic work and talk to clinical staff and community members.
-
- Patient /Family Story Project
In development
- Partnering with Long Term Care Facilities to bring Literature and Medicine: A Community Dialogue to residents and families
‘Infecting’ Hospital Culture with the ‘Spirit of the Humanities’
Growing a culture of reflective practice that focuses on humanistic medicine has been a transformation that has taken place slowly, steadily and intentionally. After just several years, I am happily seeing indications of change taking place. It is hard to walk through the hallways of our 500 bed teaching hospital in northern New Jersey without someone stopping me to chat about a book we are reading, suggest a title, comment on a poet that has recently visited or offer an insight that surfaced at a reflective writing session. This is how doctors, clinical managers, nurses and other healthcare professionals often relate to me during their day of clinical work. I consider this a clear measure of success. It indicates a hopeful shift in how the business of medicine is being done and how we are thinking of ourselves and the patients we care for. Taking even a moment in a day to connect with colleagues about the art, not the science, we see in our practice indicates an openness to explore what we are doing through the lens of the humanities. At a recent weekly clinical team meeting, the chief of medicine stopped mid sentence, ran out of the room, returning with The White Life by Michael Stein in hand. He went on to read a poignant passage about how physicians rarely experience the intimacy of caring for patients as nurses do. It was the perfect passage to get the meeting participants to recognize the essence of where our conversation was heading.
How Did This Growing Momentum of Humanities Mindfulness Begin at Our Hospital?
In 2005, I had the opportunity to participate in the first cohort of a literature and medicine seminar at the hospital. Overlook Hospital/Atlantic Health was among the first three New Jersey clinical sites invited to participate in the national Literature and Medicine: Humanities at the Heart of Health Care program supported by the Maine Humanities Council. I was still a long time tenured faculty member in an NYC community college teaching in a department completely unrelated to the medical humanities and was concurrently enrolled in the graduate program in the medical humanities at Drew University. I had extensive experience as a volunteer being with people at the end of their lives. When I was not teaching at the college I was interning with the hospital’s palliative care team. My goal was to explore palliative practices in an acute clinical care setting and transition from a long career in higher education into healthcare.
Participating in the monthly literary group especially resonated for me since I was already immersed in narrative expressions of illness through the graduate curriculum. Coming together with an interdisciplinary group of health care professionals to discuss text was a rich opportunity for me to understand the multiple voices heard within the healthcare environment. Subsequently, I more fully appreciate how this gathering of clinical and non-clinical staff successfully debunked the customary hospital hierarchy and allowed space for individuals to think and express themselves outside of their perceived professional roles.
I had also begun to write stories of patients I had been with and had the occasion to read them at professional meetings within the medical humanities community. I was asked to write a series of stories voicing the experiences of healthcare professionals at the hospital. The collection was used for the centennial celebration of the hospital’s founding. The enthusiasm for the stories by the people whose voices they echoed, and hospital community at large, was an inspiration to me. I was motivated to continue my discovery of the power of narratives and how they could be used to inform, provoke and empower people, especially as they navigated life-limiting illness and the end-of-life. This ultimately became the topic of my thesis research.
I retired from my faculty position at the college and was spending more time at the hospital. I was identifying mentors and wondering if I would ultimately find my own voice within this community of medical practitioners. By the third year of the hospital’s participation in the national literature and medicine program, I was invited to become the facilitator/scholar of the seminar. This challenged me to apply my skills as an educator in a new discipline. The seminar series has been very successful, with a waiting list of applicants, and participants who protest when we break at the completion of the six month series. We are currently contemplating to extend our current half year literature seminar throughout the academic year.
I thought it was crucial to find an effective vehicle to bring the message of palliative care to the lay community. If we were going to be effective in educating and empowering people to be advocates for the care they wanted for themselves and their loved ones at the end of life, we would have to do better than simply offering advance care planning workshops. The power, and beauty of stories and their ability to provoke change seemed clearly the way to begin opening the collective conversation about the end-of-life. With the help of a grant, this became the community seminar series, Literature and Medicine: a Community Dialogue. The series has attracted a diverse community of participants and has motivated people to take action.
With the arrival of a new chief of medicine who understands the value of humanities education and practice, new opportunities have arisen. I was asked to develop programs for resident physicians, which have been successful and extended to medical students as well. Monthly film screenings and special events have also been successful, attracting sizable numbers in attendance. With the full integration and participation of the clinical faculty, young physicians witness behaviors and attitudes modeled by their seniors that instill respect and value for the power of story. A culture that recognizes, shares and values narrative is emerging.
Moving Forward
As we move forward with our humanities education, we see opportunity for refining programs that we already offer as well as developing new programs. We are looking closely at developing a program that will be directed at eliciting patient and family stories, using those stories both as mechanisms for healing and educating. We have begun to collect some elementary data to quantify the impact and efficacy of our humanities programs upon clinical practice. Thus far, the development and implementation of these programs, has utilized very little funding. It has essentially been a grassroots initiative based on the passions of a very few individuals. However, hospital administrators have been noticing (and participating in) these activities, and there is a positive response to the work. We are now preparing to make a formal proposal to the Division of Graduate Medical Education to garner financial and institutional support to grow our programs and to partner with our affiliated hospital to expand our humanities activities.
As the vision of our programs mature, so too do we as practitioners of medical humanities. I am proud to know that I have been an agent of change in the community hospital that I work. But I am humble as well, to know that I am just learning on the shoulders of the luminaries of the medical humanities. And I am grateful.
Reference
1. William Osler. The Old Humanities and the New Science. Presidential address to the Classical Association, May 16, 1919. Online by Johns Hopkins Health System and University at http://www.medicalarchives.jhmi.edu/osler/oldhum.htm, p. 26 and p. 33.








English literature
I’ve learned something new from your post. Admirable thing you’ve written.