“This is a book about space, about language, and about death; it is about the act of seeing, the gaze,” Michel Foucault writes opening The Birth of the Clinic (p. ix).
Category: History of Medicine
Stanley B. Burns M.D. Historic Medical Photography Collection Acquired by Yale
The Stanley B. Burns M.D. Historic Medical Photography Collection was recently acquired by the Harvey Cushing/John Hay Whitney Medical Historical Library at Yale University.
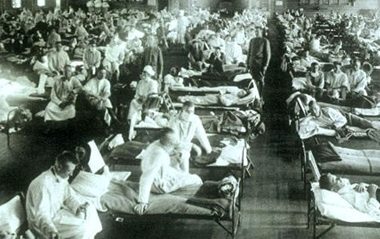
Memories of the Spanish Flu
My time spent in the army now seems to me like a long, complex dream. The events are all familiar, but you cannot be sure whether they really happened. After a very brief period of basic training in New Jersey, I was stationed in South Carolina as a physician at a small army base.
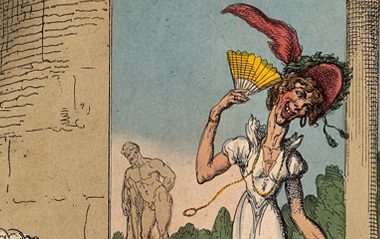
Medicine as spectacle: Public expectations of physicians as seen through art and television
If “all the worlds a stage,” then the operating theater is no different. Surgeons of the Renaissance and nineteenth and early twentieth centuries, despite the modern day medical profession’s emphasis on privacy, stoicism, and quiet dignity, were historically required, not only to heal, but to entertain.
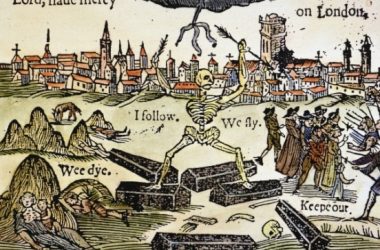
Plaguing Shakespeare
During Shakespeare’s peak writing and acting activities during the late 1500s and early 1600s, London and its environs were visited upon by plague. The plague of 1593, and the nearly continuous outbreaks from 1603–1610 had definitive effects on Shakespeare’s work (Slack 145–46; Barroll 17–18).
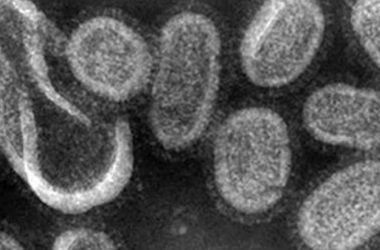
Spanish Flu Epidemic
At the end of World War I, influenza swept the globe in a devastating pandemic that affected an estimated 500 million people and killed 20 to 50 million–more than the number of deaths attributed to the recent war (up to 11 million military and up to 6 million civilians).
‘All my hurts my garden spade can heal’: Horticultural Therapy, Present & Future
Patients at the Pennsylvania Hospital in the late eighteenth century rarely enjoyed the hospital garden as a space of tranquil solitude. Just over the garden walls, past the blue wisteria and azaleas, had gathered the regular Sunday spectators who chattered about the patients who walked the lawns.
Pale Horse Pale Rider: From One Title, Two Perspectives on the Effects of the 1918 Spanish Flu Pandemic
The year 2018 marks the 100th Anniversary of the “Spanish flu” that killed tens of millions of people around the world. Among the documentaries, magazine articles, and books about the epidemic is Laura Spinny’s history
Dressing Up Tuberculosis: Carolyn A. Day’s Consumptive Chic
Unique to fashion’s allure is its mercuriality. Tastes and styles change and evolve in constant flux; what’s prosaic today might be elevated and imaginatively transformed tomorrow.