In Greek mythology, Asclepius, god of medicine, is the first physician in human history. He enters the world as his father, Apollo, pulls him from his mother’s womb.
Category: Medical Ethics
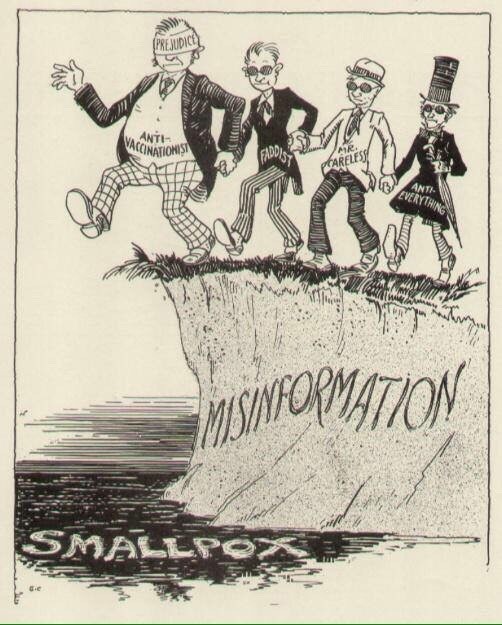
The Vaccine Project
The Rudin Fellowship in Medical Ethics and Humanities supports medical trainees at NYU School of Medicine – including medical students, residents, and clinical fellows – pursuing year-long research projects in medical humanities and medical ethics under the mentorship of senior faculty.
Two Doctors, Two Generations: Q&A with Dr. Barron Lerner
On May 6, 2014, Barron Lerner, MD, PhD, kicked off the Lerner Lectureship series with a talk that explored the evolution of medical ethics through the lens of his father’s …
The Social Construction of Cancer – Part 3
In a later visit with the homecare teams, I met Rajesh – a 29-year-old man who has been battling cancer since his teenage years.
The Social Construction of Cancer – Part 2
However, at this point, Shambu and Rohini’s story took a sharp turn. The palliative care team I was visiting with discovered that, partly because of not collectively acknowledging the extent of the disease, Shambu and Rohini had started visiting a new neighborhood private ‘ayurvedic hospital.’
The Social Constructions of Cancer
The contemporary landscape of healthcare in Delhi inspires very little confidence. The lack of public insurance, scarcity of resources and rising cost of care in the vast network of private hospitals has ensured that for much of the city’s poor, the diagnosis of cancer comes without any hope of treatment.
Walk a Mile in My Moccasins
Commentary by Amy Ellwood, MSW, LCSW; Professor of Family Medicine & Psychiatry, University of Nevada School of Medicine, Las Vegas, Nevada Communicating Through Story Storytelling has been around since the …
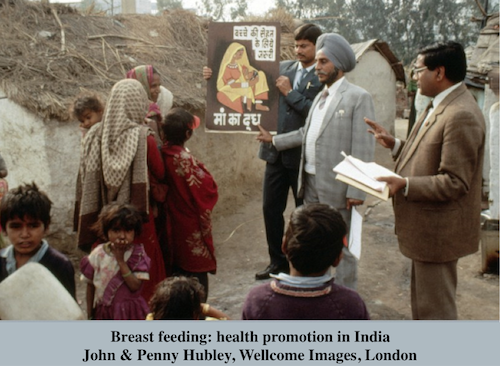
Breast Milk As Medicine And Virus: Modern Maternity And HIV/AIDS
Mothers need to be understood as neither the repositories of pure nutrition nor the potentially infectious contaminators of the young, but as materially embedded subjects whose bodies are of this world as everyone’s are.
Rescuing Sympathy
Commentary by Jack Coulehan, M.D. M.P.H., Professor Emeritus of Preventive Medicine and Fellow, Center for Medical Humanities and Bioethics, Stony Brook University, New York Many authors who write about empathy …