Commentary by Amy Ellwood, MSW, LCSW; Professor of Family Medicine & Psychiatry, University of Nevada School of Medicine, Las Vegas, Nevada Communicating Through Story Storytelling has been around since the …
Category: Program Development
English Departments and Healthcare
how professors of English might benefit from interaction with health care professionals
Physicians’ Storytelling via Webinar
The AMSA National Book Discussion Webinars offer a unique online experience between physician-authors and medical students to encourage reading beyond the medical school curriculum, both for professional development and for personal enrichment.
Sherman Alexie Wins PEN/Faulkner Award
yesterday’s announcement of the 2010 PEN/Faulkner Award for fiction, Author Sherman Alexie is the winner for fiction (War Dances, annotated in the Literature, Arts, and Medicine Database) and if you haven’t read any of his work you are missing a treat.
The “Parallel ‘Parallel Chart’”
Commentary by Hedy S. Wald, Ph.D., Clinical Assistant Professor of Family Medicine, Warren Alpert Medical School of Brown University, Providence, RI May, 2006. We treated our Doctoring small group to …
Fostering Interdisciplinary Community: A Humanities Perspective
many of us in the interdisciplinary field of medical humanities believe that it is only through a meeting of the minds between biomedicine and other fields such as literature, art, philosophy and history that we can understand the experiences of patients and providers of care (roles that almost all of us will inhabit at some point in our lives).
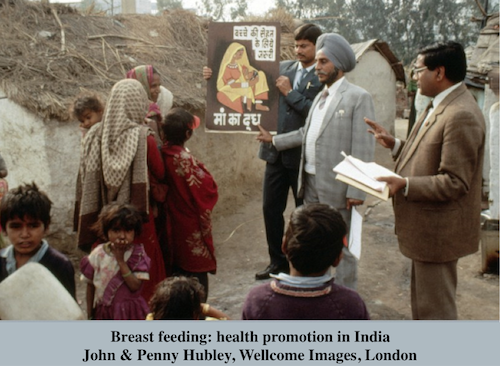
Breast Milk As Medicine And Virus: Modern Maternity And HIV/AIDS
Mothers need to be understood as neither the repositories of pure nutrition nor the potentially infectious contaminators of the young, but as materially embedded subjects whose bodies are of this world as everyone’s are.
Nurse-Poet-Writer Cortney Davis Responds To Thomas Long’s Blog On Nurse Writers
As medical schools began offering courses in the arts, humanities and creative writing as a way to increase students’ awareness of the “softer side” of caregiving, nursing programs hurried ever farther away from touch and ever closer to technology.
The Bellevue Literary Press
Commentary by Erika Goldman, Editorial Director, Bellevue Literary Press Our mission at Bellevue Literary Press is to publish books at the nexus of the arts and the sciences—with a special …