My time spent in the army now seems to me like a long, complex dream. The events are all familiar, but you cannot be sure whether they really happened. After a very brief period of basic training in New Jersey, I was stationed in South Carolina as a physician at a small army base.
Medicine as spectacle: Public expectations of physicians as seen through art and television
If “all the worlds a stage,” then the operating theater is no different. Surgeons of the Renaissance and nineteenth and early twentieth centuries, despite the modern day medical profession’s emphasis on privacy, stoicism, and quiet dignity, were historically required, not only to heal, but to entertain.
High Anxiety: Going Viral?
By Howard Trachtman, MD, Professor of Pediatrics, NYU Grossman School of Medicine and Co-editor, LitMed Database. Jenny Offill’s new book, Weather was reviewed in the New York Times and other …
End-of-Life Dreams & Visions
There’s a memorable poignancy to the beginning of your book. The nurse Nancy tells you, with gritty certitude, that a forty-year-old, HIV-positive man is terminally ill and dying
The Height of the Storm: When A Play Is as Jazz Does
The Height of the Storm, a play by Florian Zeller, can be interpreted as a fusion of two artistic genres to tell a story; in this case dramatic theater and jazz. In his essay, Russell Teagarden explores how jazz, with its variations on rhythm and themes, is embedded in the play’s structure, and how in the end, the play is as jazz does.
Saving Grace
Expecting to call in my next patient, the staff instead called me. My patient had become explosive, thrashing about in the waiting area, prompting a call to 911.
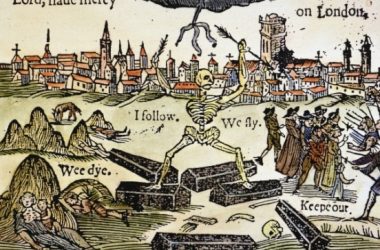
Plaguing Shakespeare
During Shakespeare’s peak writing and acting activities during the late 1500s and early 1600s, London and its environs were visited upon by plague. The plague of 1593, and the nearly continuous outbreaks from 1603–1610 had definitive effects on Shakespeare’s work (Slack 145–46; Barroll 17–18).
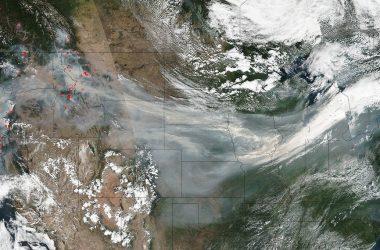
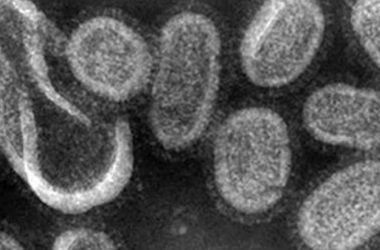
Spanish Flu Epidemic
At the end of World War I, influenza swept the globe in a devastating pandemic that affected an estimated 500 million people and killed 20 to 50 million–more than the number of deaths attributed to the recent war (up to 11 million military and up to 6 million civilians).
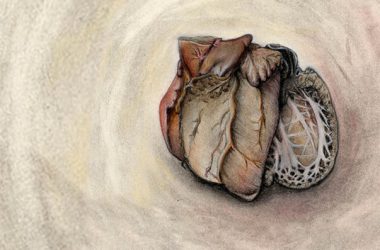
Announcing the Art & Anatomy Website
The Master Scholars Program in Humanistic Medicine (MSPHM) at NYU Grossman School of Medicine is thrilled to announce the launch of a new website: ArtandAnatomy.com.